Bed sores, also known as pressure ulcers or decubitus ulcers, are a common and potentially serious condition that can affect individuals who are bedridden, infirm, debilitated and malnourished, or have limited mobility. According to the bed sore definition, these ulcers crop up due to prolonged pressure on the skin, often in areas where bones are close to the skin surface, such as the heels, hips, lower back, and elbows. The constant pressure restricts blood flow to the affected area, leading to tissue damage and painful sores.[1]
Recognizing the symptoms of bed sores is crucial for early detection and intervention. In the initial stages, the affected area may appear red and fail to blanch when pressed. The skin may darken or develop blisters and open wounds as the condition progresses, increasing the risk of infection and complications [2] This article will explore the primary bed sore causes, symptoms, various bed sore grading, bed sores treatment, and bed sore prevention measures.
What are the symptoms of bed sores?
Redness:
Initially, the affected area may appear red and may not turn pale when pressed.
Blisters or sores:
Open wounds, blisters, foul odor, or skin breakdown may occur.
Increasing pain:
The area may be painful to the touch, with erythema, edema, and heat of the peri-wound area.
Wound drainage:
Fluid or pus may be present.
Fever:
The patient may exhibit fever, chills, and malaise, especially if the initial local wound is not treated correctly. [5]
What are the causes of bed sores?
Among the main bed sore causes are:
Pressure:
Prolonged pressure on the skin and soft tissues can restrict blood flow, leading to tissue damage.
Moisture:
Excessive exposure to moisture, such as sweat, blood, urine, or feces, especially in patients with limited mobility over long periods, can lead to the likelihood of bed sores. [3]
Friction:
Rubbing or friction between the skin and another surface can damage the skin.
Immobility:
Patients with profound immobility are also prone to developing bed sores.
Shear:
This is a significant cause of bed sores, especially in areas where the body is often supported when in a particular position, such as lying or sitting. [4]
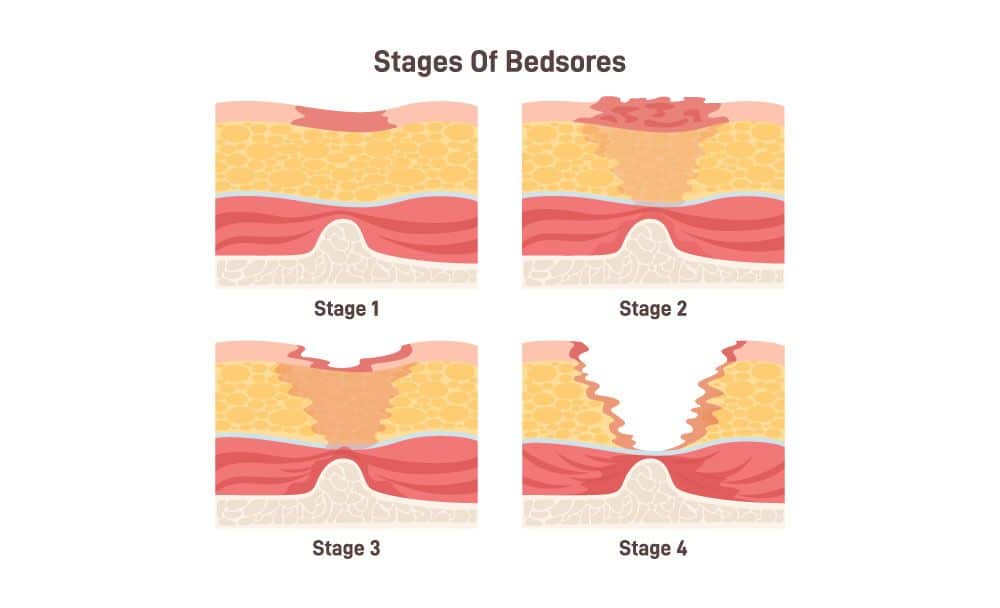
What are the various stages of bed sores?
There are essentially four main bed sore stages:
Stage 1:
Pressure-related changes with redness, intact skin, changes in temperature, and a sensation of pain and itching are the first of the four bed sore stages.
Stage 2:
The second of the four bed sore stages is partial-thickness skin loss involving the epidermis and dermis.
Stage 3:
Full-thickness skin loss occurs, and it extends to the subcutaneous tissue.
Stage 4:
Full-thickness skin loss with extensive tissue damage, exposing muscle, tendon, or bone happens in this type of bed sores. [2]
How can bedsores be treated?
There are various methods of bed sores treatment that one can follow:
Relieve pressure:
Frequent repositioning, using specialized cushions or mattresses, and avoiding pressure on the affected area can be one of the main bed sores treatments.
Improve nutrition:
Ensure a diet rich in protein, Vitamin C, Iron, and Zinc.
Clean and dress the wound:
Keep the wound clean, use appropriate dressings, and manage any infection.
Debridement:
Removing dead or necrotic tissue to promote healing is also a bed sores treatment.
Wound care: Use appropriate products to moisten the wound and provide a favorable healing environment.
Medications:
Yet another bed sores treatment is the use of antibiotics, and this may be prescribed if an infection is present.
Surgical interventions:
In severe cases, surgical procedures such as skin grafts or flap reconstruction may be necessary as the only form of bed sores treatment. [4]
How can you prevent bed sores?
Some of the bed sore prevention that one can adopt are:
Regular repositioning:
Change positions periodically, use support surfaces, including static and dynamic devices, or use specialized equipment to relieve pressure.
Good nutrition:
Maintain a balanced diet and stay well-hydrated to promote healthy skin and prevent bed sores.
Skincare:
Keep the skin clean with isotonic saline, avoid excessive moisture, as well as excessive dryness as inflicted by hot water and soap, and avoid excessive friction or shearing.
Use supportive devices:
Utilize pressure-relieving cushions, specialized foam mattresses, and low air-loss beds.
Regular assessment and good nursing:
Monitor high-risk individuals for early signs of bed sores. [2]
FAQs
1. What is the best Ayurvedic treatment for bed sores on buttocks?
Among the best Ayurvedic treatment for bed sores on buttocks are:
1. Dust the area with a fine powder of Tankana bhasma or purified borax, which brings down the discharge and helps dry up the wound causing your bed sores.
2. Prepare Triphala kwath, a water decoction at home, to wash the wound before dressing it.
3. You can use ropana taila, jatyadi oil, and vranabhairava taila as an effective treatment for bed sores on buttocks.
4. Apply panchaguna taila to reduce pain, swelling, and ulceration.
2. What are some of the common sites of pressure ulcers?
Some common sites of bed sores include the tailbone or buttocks, spine, shoulder blades, and the backs of legs and arms that usually rest against a chair. It may also happen in bedridden patients on the sides or back of the head, hip, lower back, heels, ankles, or the skin behind the knees.
3. When should you ask for medical help in case of bed sores?
If no improvement is visible in the status of your bed sores even 24 to 48 hours after changing positions or relieving the pressure in the area, you should get medical help.
Conclusion
It is essential to focus on and emphasize the importance of early intervention in bed sores as they can progress rapidly and become difficult to treat. Seeking medical attention and guidance from healthcare professionals is crucial for proper diagnosis, personalized treatment plans, and ongoing care. This article is an attempt on our part to spread awareness about bed sores, know the bed sore meaning, its symptoms, bed sore causes, bed sore grading, bed sores treatment options, and bed sore prevention strategies. This way, we can work towards reducing the prevalence of these debilitating ulcers and improving the overall well-being of those at risk.
Disclaimer:
This article is written from a health and wellness perspective and is not medical advice. Kindly seek the help of a certified medical practitioner before initiating any treatment.
References:
- Bedsores Management: Efficiency Simulation of a New Mattress Design
- Bedsores: “Top to bottom” and “bottom to top”
- The knowledge of bedsores prevention among Health and Nursing Department students of Medical University of Białystok
- Pressure ulcers: Current understanding and newer modalities of treatment
- Pressure Ulcer