This article is reviewed by Dr. Jyoti Lakhani.

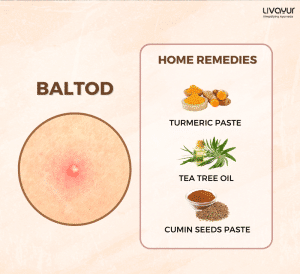
Paronychia is a prevalent skin infection that affects the area surrounding the toenail or fingernail. The condition is classified into two types: acute and chronic (1).
Find out everything you need to know about paronychia, including its causes, symptoms, diagnosis, prevention, and treatment options, in this article.
Types, Causes & Risk Factors of Paronychia (1)
Acute paronychia
This type of paronychia usually appears suddenly and causes a very painful area of swelling, warmth, and redness around a fingernail or toenail. It is typically caused by a bacterial infection after nail injury.
Some factors that may increase the risk of getting nail injuries and acute paronychia include:
- Overaggressive manicuring
- Cutting or tearing the cuticle
- Biting the edges of the nails or skin around the nails
- Picking at the skin near the nails
- Sucking on the fingers
Chronic Paronychia
Inflammation is the root cause of this variety of paronychia, which typically progresses gradually and results in swelling, tenderness, and redness of the skin surrounding the nails.
Some factors that may increase the risk of developing chronic paronychia include:
- Exposure to water, chemicals, or substances to which they are allergic
- Jobs that constantly expose the hands to water, chemicals, or substances
- Diabetes
- Candida (yeast) infection in some cases
Symptoms of Paronychia (1)
The symptoms of paronychia depend on the type of paronychia you have.
Acute paronychia usually affects only one nail. Some of the common symptoms of acute paronychia include:
- Throbbing pain
- Redness, warmth, and swelling in the skin around the nail
- A minor accumulation of pus beneath the nail or in the skin surrounding the nail
Chronic paronychia typically affects several nails on the same hand at the same time. Some of the common symptoms of chronic paronychia include:
- Tender, red, and mildly swollen area around the nail
- Missing cuticle
- Moist or “boggy” skin around the nail
If you experience any of these symptoms, see a healthcare professional for proper diagnosis and treatment.
Diagnosis of Paronychia (1)
Paronychia can usually be self-diagnosed by examining the affected area for symptoms of paronychia.
However, if you have diabetes, are experiencing severe symptoms such as pus, fever, or severe pain, or have several affected fingers or toes, you may require evaluation by a doctor.
In some cases, your doctor may also take your pus sample to diagnose bacterial or fungal infection.
Modern Treatment of Paronychia (1)
The type of treatment you need depends on the type of paronychia you have.
Acute Paronychia
If you have acute paronychia, you can try soaking your finger or toe in warm water for at least 15 minutes, two to four times a day. However, if you don’t see any improvement in your condition or your condition worsens, consult a doctor.
In most cases, doctors will prescribe an oral antibiotic. However, if pus has accumulated near the nail, your doctor may also numb the area and drain the pus. In severe cases, a small part of your nail may also be removed to ensure the area drains completely.
Chronic Paronychia
If you have chronic paronychia, it is essential to consult a doctor for treatment. Your doctor may recommend a topical corticosteroid ointment or cream, with or without a topical antifungal agent. Your doctor will also ask you to keep your skin clean and dry and wear gloves when exposed to any irritants.
In severe cases, your doctor may also prescribe antifungal drugs or steroids to treat the condition.
Treatment of Paronychia in Ayurveda
Paronychia can be related to a condition mentioned in Ayurveda by the name of Kshudra Roga Kunakha. Kunakha refers to the common physical sign of nail disease, which is discoloration of the nail (2).
Here are some key herbal formulations used in Ayurveda to address paronychia:
Jatyadi Oil
Known for its Kledahara (moisture-absorbing) properties, Jatyadi oil exhibits Vrana Shodhaka (wound-cleansing) and Vranaropaka (wound-healing) effects (2).
Kaishor Guggulu
This herbal formulation possesses Rakta Prasadak (blood-purifying) properties. By promoting vasodilation and correcting Pitta Dushti (imbalance), it aids in reducing inflammation by providing fresh blood (2).
Gandhaka Rasayan
With its Pitta Shamak (Pitta-reducing) nature, Gandhaka Rasayan acts as an anti-inflammatory agent. It helps maintain balance among the Vata, Pitta, and Kapha Doshas and possesses antibacterial, antiviral, and antimicrobial properties that help purify the blood, enhance immunity and fight infections (2).
Sukshma Triphala Vati
This proprietary medicine combines Kajjali and Triphala, offering anti-inflammatory and antibiotic effects. Its high penetration capacity at the cellular level corrects the infection and inhibits further necrosis of local tissue (2).
Capsule Cutis
This herbal formulation inhibits inflammatory actions and supports the natural healing process of the affected area (2).
Panchnimb Churna
Acclaimed for its antibacterial and antifungal properties, Panchnimb Churna is beneficial in the treatment of paronychia (2).
Ayurveda also recommends using therapies to treat paronychia, such as:
Jalaukavcharan (Leech Therapy)
Jalaukavcharan, a form of Raktamokshan (bloodletting) therapy, helps reduce pus formation and provides relief from swelling (3).
Vrana Dhoopana and Vrana Ropana Tail Pichu
Vrana Dhoopana involves fumigation with medicinal smoke directed towards the affected area whereas Vrana Ropana Tail Pichu is the application of a medicated oil-soaked cotton swab on the affected area, covered with a bandage for a specific duration (3).
The most commonly used herbs in this therapy include Haridra (turmeric), Musta, Vacha, Yashtimadhu (liquorice) and Guggul (Commiphora wightii) (3).
Vrana Dhoopan Karma is usually performed after Jalaukavcharan and then followed by Vrana Ropana Tail Pichu (3).
Disclaimer: Always consult with a qualified Ayurvedic practitioner before using any herbal formulation or therapy for paronychia.

How Long Does a Paronychia Last? (1)
The length of time for a paronychia to heal depends on the type of paronychia you have.
Generally, with appropriate treatment, acute paronychia can be cured within a period of 5 to 10 days. However, treating chronic paronychia can take longer, possibly several weeks, with the use of antifungal medication.
Keep in mind that paronychia can recur even after proper medical therapy, especially if the skin around the nail is re-injured or the nail area becomes moist again.
Prevention of Paronychia (1)
The best way to prevent paronychia is to take good care of your nails and avoid injury to the skin around them.
Here are some tips to help you prevent paronychia:
- Keep your hands and feet clean and dry all the time.
- Wear rubber gloves lined with absorbent cotton if your hands are regularly exposed to water or chemicals.
- Avoid cutting your cuticles or pushing them back.
- Avoid biting your nails or picking at the surrounding skin.
- If you have diabetes, regulate your blood sugar levels by eating a healthy diet and taking prescribed medications.
The Final Takeaway
Paronychia is a common infection that affects the skin around the nails of the fingers or toes. It can be acute or chronic, and its causes, symptoms, and treatment options depend on the type.
However, proper care of the nails and avoiding injuring the skin around them can prevent paronychia.
Remember, if you experience any symptoms of paronychia, seek medical attention promptly to avoid complications.
FAQs
1. How can I differentiate between acute and chronic paronychia?
Acute paronychia appears suddenly and causes pain, swelling, and redness around the nail, while chronic paronychia progresses gradually, resulting in tenderness, redness, and swelling of the skin surrounding the nails.
2. When should I seek medical attention for paronychia?
If you experience symptoms of paronychia, such as pain, swelling, redness, or pus, it is important to seek medical attention promptly to avoid complications.
3. How long does it take for paronychia to heal?
Acute paronychia can typically be cured within 5 to 10 days with proper treatment. Chronic paronychia may take longer, possibly several weeks, especially when antifungal medication is used. However, recurrence can happen if the skin is reinjured or becomes moist again.
References
- https://www.health.harvard.edu/a_to_z/paronychia-a-to-z
- https://www.researchgate.net/publication/340612794_Contribution_of_Ayurveda_for_management_of_paronychia_A_case_report
- https://www.researchgate.net/publication/364629923_An_effective_use_of_Ayurvedic_management_in_case_of_Nail_Bed_Infection-_A_case_report