Gestational diabetes is the most common form of complication and a type of diabetes that occurs during pregnancy. It is known to have short-term as well as long-term effects on the mother as well as her offspring. The condition consists of high blood sugar levels that develop during pregnancy in women who are overweight, are childbearing at a late age, have a previous history of gestational diabetes mellitus, or have a family history of type 2 diabetes mellitus. [1]
While gestational diabetes treatment improves immediate pregnancy outcomes, such as reducing excess fetal growth and adiposity and pregnancy-related hypertensive disorders, it has the potential to increase the risk of long-term complications, such as obesity, impaired glucose metabolism, as well as cardiovascular disease, in both the mother and the child. Although it requires careful management to ensure the health of both the mother and the baby, long- term follow- up continues to be a challenge due to the limited implementation of preventive strategies in most parts of the world. [1] In this comprehensive guide, we will explore gestational diabetes mellitus definition, gestational diabetes symptoms, gestational diabetes causes, and treatment options for gestational diabetes that will help in dealing with it better.
Meaning of Gestational Diabetes
Gestational diabetes mellitus definition states that it is a temporary phase of diabetes that develops during pregnancy. It is generally detected in the late second trimester, which is between the 13–26 completed weeks of gestation, or early in the third trimester, which is between 27–40 weeks, and resolves following delivery. [1] It is a result of glucose intolerance, which can interfere with the body’s ability to effectively use insulin. Insulin is a kind of hormone that helps regulate blood sugar levels. When gestational diabetes occurs, the pancreas may not produce enough insulin or use it efficiently, leading to elevated blood sugar levels. [4]
Symptoms of Gestational Diabetes
Gestational diabetes may not present with obvious symptoms, and many women may not even be aware they have the condition. However, some common signs and gestational diabetes symptoms include:
Causes of Gestational Diabetes
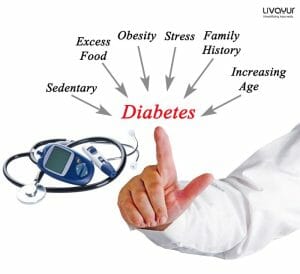
Gestational diabetes causes are usually attributed to hormonal and physiological changes during pregnancy. Some factors that may contribute to the development of gestational diabetes include:
Insufficient insulin production:
One of the common gestational diabetes mellitus causes is that there may not be adequate production of insulin to overcome the insulin resistance caused by pregnancy hormones.
Genetic predisposition:
Women with a family history of diabetes or who have previously had gestational diabetes are more prone to developing gestational diabetes.
Excess weight:
Being overweight or obese before pregnancy increases the risk of developing gestational diabetes.
Age:
Advanced maternal age puts women at a higher risk of gestational diabetes.
Other factors:
Lifestyle may be one of the biggest gestational diabetes causes and may include unhealthy dietary practices, excessive smoking, high exposure to persistent organic pollutants, Polycystic ovary syndrome, previous history of gestational diabetes mellitus, as well as a male fetus. [1]
Diagnosis of Gestational Diabetes

Gestational diabetes is typically diagnosed between the 24th and 28th weeks of pregnancy through a glucose screening test such as the glucose challenge test and the oral glucose tolerance test (OGTT). If the initial test results indicate elevated blood sugar levels, a follow-up glucose tolerance test may be conducted to confirm the diagnosis. [3]
Treatment and Management
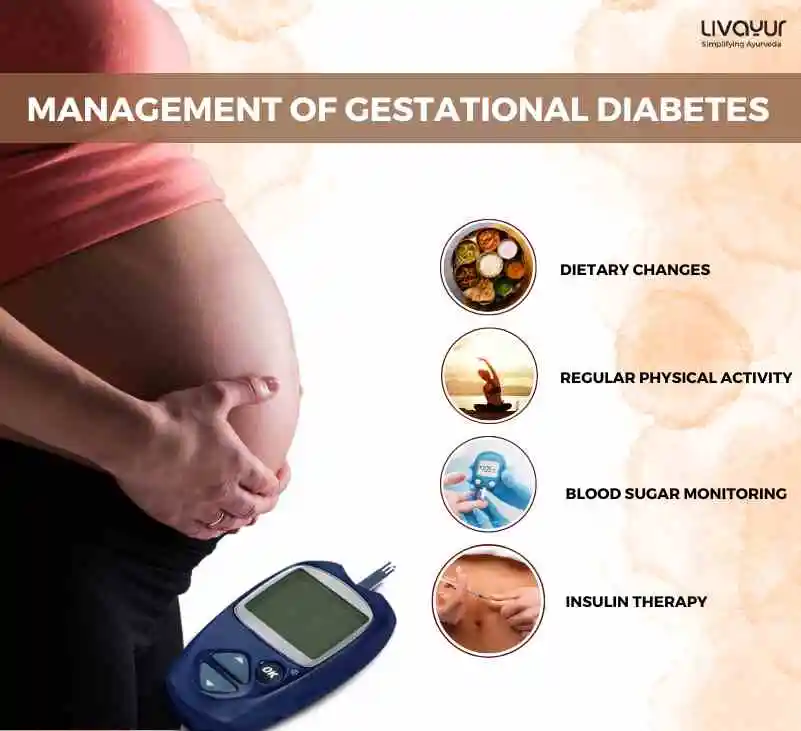
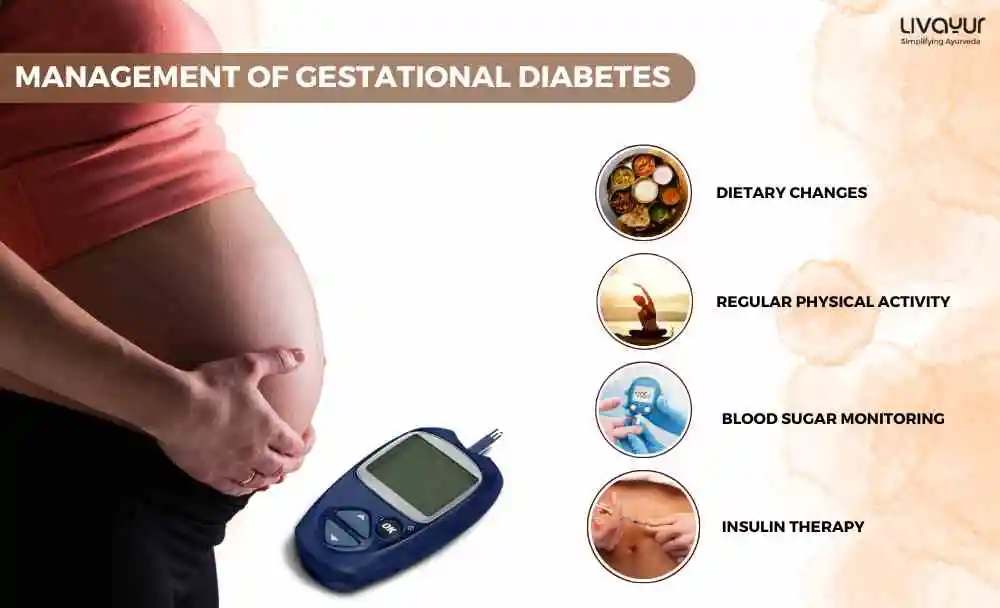
The management of gestational diabetes mellitus focuses on controlling blood sugar levels to ensure a healthy pregnancy and minimize risks for both the mother and the baby. Gestational diabetes treatment options may include:
Dietary changes:
A registered dietitian can help develop a balanced meal plan that ensures adequate nutrition and achieves glycemic goals while controlling blood sugar levels without inducing weight loss or excessive weight gain. This may involve consuming regular small meals of slowly absorbed carbohydrates and eating fruits, vegetables, and low-fat dairy foods.
Regular physical activity:
Getting involved in regular physical activities, as advised by a healthcare provider, can help lower blood sugar levels. Suitable activities may include walking, aqua aerobics, or prenatal exercise classes.
Blood sugar monitoring:
Women with gestational diabetes are often required to monitor their blood sugar levels regularly. This acts as a gestational diabetes treatment to track the effectiveness of dietary changes and identify any necessary adjustments to the treatment plan.
Insulin therapy:

If blood sugar levels remain high despite dietary and lifestyle modifications, insulin therapy may be recommended. Insulin is administered through injections to help regulate blood sugar levels. [2]
Potential Risks and Complications
Gestational diabetes mellitus, if left unmanaged, can lead to various complications for both the mother and the baby. Some potential risks include:
Preeclampsia:
Gestational diabetes mellitus increases the risk of developing preeclampsia, a condition that can harm both the mother and the child. [5]
Risks of perinatal complications:
There may be an increased risk of delayed intrauterine fetal development or macrosomia, which can lead to complications during delivery and increase the likelihood of cesarean section, bradytocia due to macrosomia, and induction of childbirth. [2]
Risk of lifestyle-related diseases:
Babies born to mothers with gestational diabetes mellitus may develop the risk of lifestyle-related diseases after birth. [2]
Type 2 diabetes risk:
Women who have had gestational diabetes mellitus are at a higher risk of falling prey to type-2 diabetes later in life. [2]
FAQs
- How can postpartum care help in dealing with gestational diabetes mellitus?
After delivery, the mother’s blood sugar levels usually return to normal. However, gestational diabetes for pregnant women entails that they should continue monitoring their blood sugar levels and undergo follow-up testing. Adopting healthy lifestyle measures, such as maintaining a balanced, healthy diet and getting involved in regular physical activity, can lower the chances of developing type 2 diabetes in the future.
- How can you treat gestational diabetes mellitus through Ayurveda?
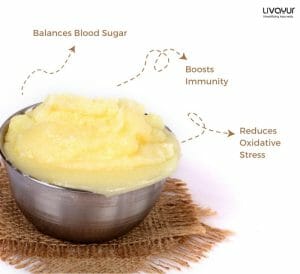
There are some common Ayurveda remedies for gestational diabetes, such as:
Gurmaar: Also known as The Sugar Killer, this contains gymnemic acid molecules, which have an anti-diabetic effect.
Karela: Commonly known as bitter gourd, this has anti-diabetic properties and also contains many other micronutrients, which are crucial in preventing the complications.
Vizaysaar: This is obtained from the bark of a tree and is very useful for diabetes.
Saptrangi: This is a tree whose bark is immersed in water and then drunk by a patient suffering from diabetes.
Tulsi: Also known as Ocimum sanctum, this plant has tremendous medicinal properties, including treating and reducing blood sugar.
Ashwagandha: This is another great remedy for diabetes.
- What do you understand by gestational diabetes range?
Gestational diabetes range indicates a blood sugar level of 190 milligrams per deciliter (mg/dL), or 10.6 millimoles per liter (mmol/L). In case the blood sugar level is below 140 mg/dL (7.8 mmol/L), it usually means that you are within the standard range on a glucose challenge test.
Conclusion
Gestational diabetes is a temporary diabetic condition that occurs during pregnancy and requires careful management to ensure the well-being of both the mother and the baby. By adhering to a nutritious diet, engaging in regular physical activity, monitoring blood sugar levels, and, if necessary, using insulin therapy, women with gestational diabetes can effectively manage their sugar levels and minimize potential complications. Knowing all about gestational diabetes symptoms and with proper gestational diabetes symptoms and ongoing care, most women with gestational diabetes deliver healthy babies and experience a healthy postpartum period.
Disclaimer: This article is written from a health and wellness perspective only and is not a piece of medical advice. Kindly seek the help of a certified medical practitioner before initiating any treatment.
References:
- Gestational diabetes mellitus
- A REVIEW ARTICLE-GESTATIONAL DIABETES MELLITUS
- Gestational Diabetes
- Symptoms & Causes of Gestational Diabetes
- Gestational diabetes: Overview
Manage Diabetes With The Knowledge Of Ayurveda (Download Ebook)